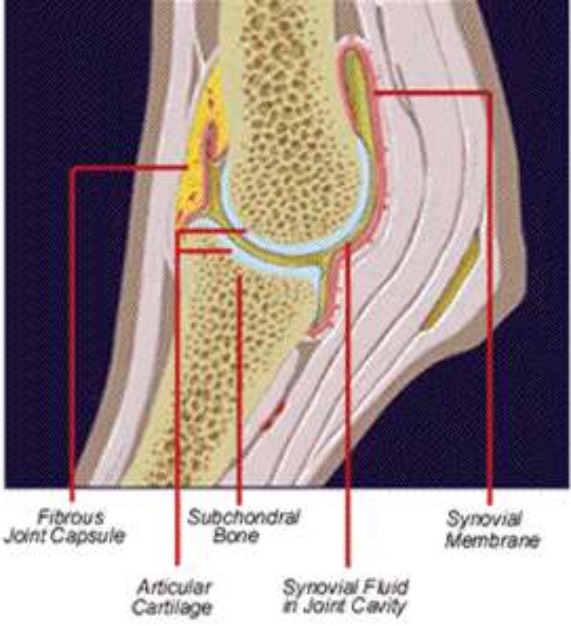
To understand how lameness occurs, you must be familiar with healthy joint function and how inflammation causes damage to the joint. Three components are most important to maintaining normal joint action: the joint capsule, synovial fluid (also called synovia) and articular cartilage.
The joint capsule is fibrous tissue that connects the bones of the joint and serves to contain the joint fluid. The inner surface of the joint capsule is lined with the synovial membrane, a connective tissue thick with blood vessels that produces synovial fluid.
Synovial fluid consists of blood plasma components and sodium hyaluronate. This fluid is clear, lubricating and semi-solid. When a joint is under physical load, the amount of synovial fluid increases in the stressed joint. Normal volume is reached after a few hours' rest.
Articular cartilage covers the bone ends and is subjected to greater mechanical stress than any other joint tissue. The condition of the articular cartilage is a determining factor when assessing a joint's potential for working properly. Articular cartilage consists of collagen, proteoglycans, sodium hyaluronate and a great deal of water (60 to 80 percent).
Collagen, which is about 50 percent of the dry material of the cartilage, absorbs, equalizes and dampens the mechanical load put on the articular cartilage. Adult animals have a limited ability to produce new collagen. This limited capacity for healing contributes to the seriousness of arthritis, particularly for high-performance animals. Proteoglycans add elasticity to articular cartilage.
Water molecules, bound by the network of sodium hyaluronate chains, help maintain the health and function of the joint.
Cartilage cells, called chondrocytes, are somewhat sparsely located in the cartilage mass. They have neither blood vessels nor lymph vessels within easy reach for their nutrition.
The synovial fluid provides a supply of nutrients through a natural pumping action as the cartilage is loaded and unloaded. When the joint is under load, the elastic cartilage, including the network of sodium hyaluronate, compresses. Part of its liquid content, including degraded products, is expelled into the synovial fluid. When the joint is relieved, the cartilage works to regain its volume, drawing in liquid and nutrients, especially glucose. This exchange of nutrients and waste is required to maintain functional cartilage, because the joint does not have access to nutrients from the bloodstream.
Should the joint suffer trauma, inflammation usually begins in the synovial membrane. Inflammation of the synovial membrane is called synovitis. When a joint is inflamed, leukocytes (white blood cells) are activated and migrate into the joint cavity, where they release destructive free radicals and proteolytic enzymes. These enzymes and free radicals erode the tissue surrounding the joint and damage the articular cartilage. The damage may be permanent, because articular cartilage has only a limited capacity for healing.
Research has shown that degradation of the proteoglycans occurs in the inflammatory process and is a significant part of joint degeneration. As the proteoglycans degrade and leave the cartilage, the elasticity of the cartilage also decreases. Consequently, the pumping mechanism that carries the nutrients between the synovial fluid and the chondrocytes becomes less efficient. With fewer nutrients, the chondrocytes cannot replenish the cartilage matrix as quickly as it is degraded. If this process is not stopped in time, the degeneration proceeds to a point of no return. Early diagnosis, swift treatment and rest are crucial.